Fig
Listening Guide for CD Track 2, “La Comparsa” 0:00-0:05 Initial solo statement of the repeated left-hand figure that serves as the structural basis of the composition. It is played softly, as if the music were at a distance. As mentioned, the left-hand figure is a “ clave -d” rhythm consisting of an initial syncopated half over one measure and a straighter half over the next. It outlin
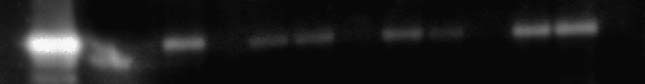 Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.
Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.