Health innovation systems
HEALTH INNOVATION SYSTEMS IN DEVELOPING COUNTRIES Strategies for Building Scientific and Technological Capacities John Mugabe NEPAD Office of Science and Technology WORKING DRAFT Health Innovation Capacities of Developing Countries INTRODUCTION There is a growing recognition that the extent to which developing countries will be able to reduce the burden of disease an
 European Heart Journal Advance Access published November 29, 2006
European Heart Journal Advance Access published November 29, 2006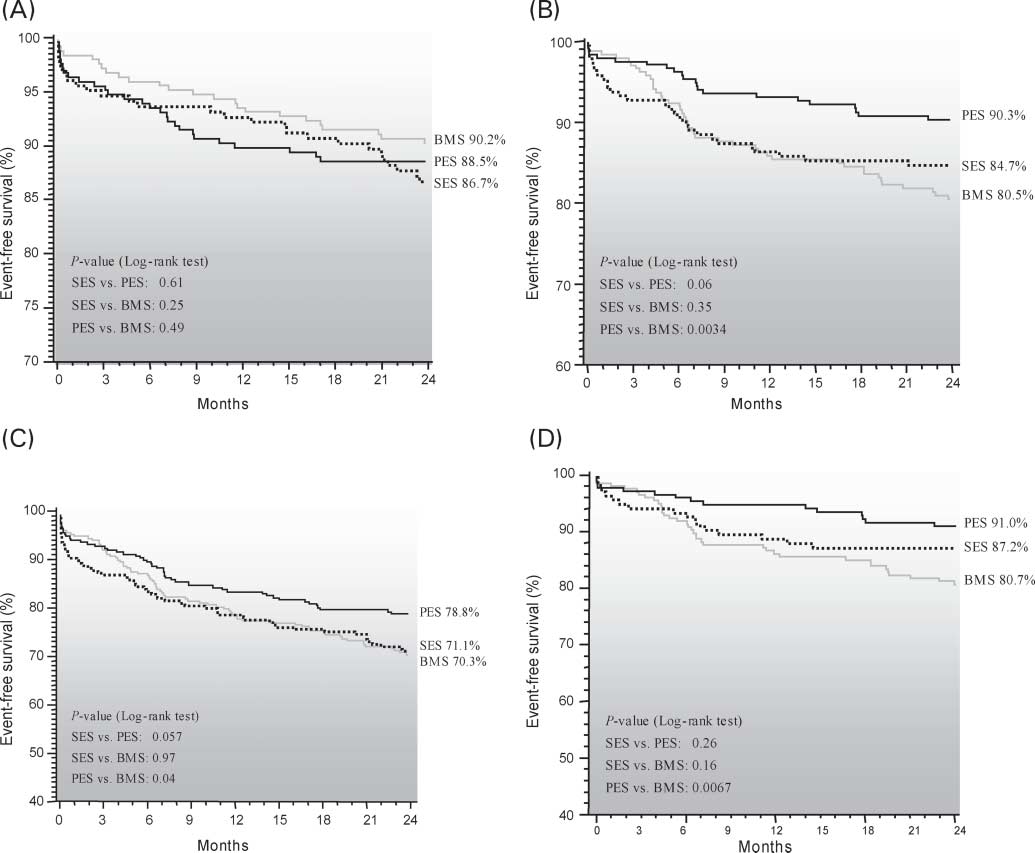 Two-year cumulative incidence of mortality (A), TVR (B), major adverse cardiac events (C), and TVR in NIDDM (D), in patients treated with BMS, SES, or
the BMS patients, vs. 18.2% and 14.7% of the SES and PES
died, seven presented with an MI, and 12 patients were
patients, respectively (P ¼ 0.33 SES vs. PES). TLR was per-
still on dual-antiplatelet therapy at the time of the event.
Two-year cumulative incidence of mortality (A), TVR (B), major adverse cardiac events (C), and TVR in NIDDM (D), in patients treated with BMS, SES, or
the BMS patients, vs. 18.2% and 14.7% of the SES and PES
died, seven presented with an MI, and 12 patients were
patients, respectively (P ¼ 0.33 SES vs. PES). TLR was per-
still on dual-antiplatelet therapy at the time of the event.